Peptide is a kind of biochemistry material with wide range function and there are many kinds of peptide in drug world. Among these medicinal peptide products, Cyclosporine A becomes a high-profile star because of its unique immune inhibition.
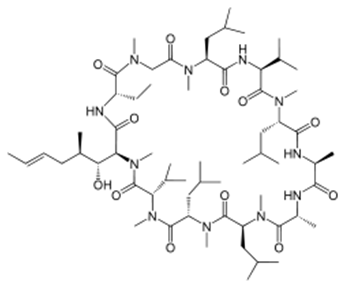
Cyclosporine A (often shortened to CsA) is an immunosuppressant drug widely used in organ transplantation to prevent rejection. It reduces the activity of the immune system by interfering with the activity and growth of T cells. It was initially isolated from the fungus Tolypocladium inflatum (Beauveria nivea), found in a soil sample obtained in 1969 from Hardangervidda, Norway, by Hans Peter Frey, a Sandoz biologist. Most peptides are synthesized by ribosomes, but ciclosporin is a cyclic nonribosomal peptide of 11 amino acids and contains a single D-amino acid, which are rarely encountered in nature [1].
The immunosuppressive effect of ciclosporin was discovered on 31 January 1972 by employees of Sandoz (now Novartis) in Basel, Switzerland, in a screening test on immune suppression designed and implemented by Hartmann F. Stähelin. The success of ciclosporin in preventing organ rejection was shown in kidney transplants by R.Y. Calne and colleagues at the University of Cambridge, and in liver transplants performed by Thomas Starzl at the University of Pittsburgh Hospital. The first patient, on 9 March 1980, was a 28-year-old woman. Ciclosporin was subsequently approved for use in 1983.
Ciclosporin is approved by the FDA to prevent and treat graft-versus-host disease in bone-marrow transplantation and to prevent rejection of kidney, heart, and liver transplants. It is also approved in the US for the treatment of rheumatoid arthritis and psoriasis and as an ophthalmic emulsion for the treatment of dry eyes. In addition to these indications, ciclosporin is also used in severe atopic dermatitis, Kimura’s disease, pyoderma gangrenosum, chronic autoimmune urticaria, and, infrequently, in rheumatoid arthritis and related diseases, although it is only used in severe cases. Ciclosporin has also been used to help treat patients with acute severe ulcerative colitis that do not respond to treatment with steroids. This drug is also used as a treatment of posterior or intermediate uveitis with noninfective etiology.
In medicine, the most important effect of ciclosporin is to lower the activity of T cells and their immune response. Ciclosporin binds to the cytosolic protein cyclophilin (immunophilin) of lymphocytes, especially T cells. This complex of ciclosporin and cyclophilin inhibits calcineurin, which, under normal circumstances, is responsible for activating the transcription of interleukin 2. In T-cells, activation of the T-cell receptor normally increases intracellular calcium, which acts via calmodulin to activate calcineurin. Calcineurin then dephosphorylates the transcription factor nuclear factor of activated T-cells (NFATc), which moves to the nucleus of the T-cell and increases the activity of genes coding for IL-2 and related cytokines. Ciclosporin prevents the dephosphorylation of NF-AT by binding to cyclophilin. It also inhibits lymphokine production and interleukin release and, therefore, leads to a reduced function of effector T-cells. It does not affect cytostatic activity. Cyclosporine affects mitochondria by preventing the mitochondrial permeability transition pore from opening, thus inhibiting cytochrome c release, a potent apoptotic stimulation factor. This is not the primary mechanism of action for clinical use, but is an important effect for research on apoptosis [2]. In recent years, the researchers pay more and more attention to the side effect of Cyclosporine. For example, Chronic cyclosporine A (CsA) nephrotoxicity (CCN) is an important cause of chronic renal dysfunction with no effective clinical intervention. Renal cell apoptosis was an important feature of CCN and an important factor of renal dysfunction. First, CsA could upregulate Fas/Fas ligand, downregulate Bcl-2/Bcl-XL, and increase caspase-1 and caspase-3. Second, it could induce oxidative stress and damage the antioxidant defense system. Third, it could increase endoplasmic reticulum stress protein in a dose- and time-dependent manner. Fourth, CsA could impair the urine concentration and decrease the expression of hypertonicity-induced genes. Fifth, CsA-induced renal cell apoptosis was significantly decreased by blocking the angiotensin II type 1 receptor using losartan. The in vivo mechanisms for CCN are more complex than those found in vitro. CsA can induce renal cell apoptosis using five pathways in vivo and activated caspases might be the ultimate intersection of these pathways and the common intracellular pathway mediating apoptosis. [3]
Today, Cyclosporine has been used in clinic for a long time, and the research on its molecular mechanism is more and more hot. Karebay can synthetic Cyclosporine with biotin and fluorescent labels, so that scientists can knew more details about its molecular mechanism. karebay (www.karebaybio.com) has a professional team devoted to peptide products synthesis and development. We offer high-quality peptide synthesis products for sale around the world, including over 1,000 catalog peptides, and nearly 100 pharmaceutical peptides and cosmetic peptides products.
References [1] Cantrell DA, Smith KA (1984). “The interleukin-2 T-cell system: a new cell growth model”. Science. 224 (4655): 1312–1316. [2] Mott JL, et al. (July 2004). “Cardiac disease due to random mitochondrial DNA mutations is prevented by cyclosporin A”. Biochem. Biophys. Res. Commun. 319 (4): 1210–5. [3] Xiao Z,et al. Mechanisms of cyclosporine-induced renal cell apoptosis: a systematic review. Am J Nephrol. 2013;37(1):30-40.